Microfluidic technology came to prominence in the 1990s in the aftermath of the Cold War, in response to the threat of chemical and biological weapons. These were considered a major military and terrorist threat, so the US Defense Advanced Research Projects Agency (DARPA) invested heavily in field-deployable microfluidic systems capable of rapidly detecting biological agents, so that any protective response could be swift.
That might have been the first significant breakthrough for microfluidics, but the technology shares a much longer lineage with microelectronics. Indeed, it was originally hoped that the technologies that made microelectronics such a success as early as the mid-20th century would translate directly to microfluidics. Due partially to different material requirements and the difficulties of working with fluids on the micro to picolitre range, that wasn’t the case. Instead, it was the explosion of genomics in the 1980s and the development of high-throughput DNA sequencing that laid the groundwork for the rapid growth of microfluidic technology. In the past 25 years, progress in the field of microfluidics has made it important for commercial product development across several industries. This has been especially true in the field of diagnostics.
Despite developments within it leading to many devices that significantly outperform their predecessors, as well as the creation of completely novel technologies, microfluidics is still considered a discipline in adolescence. This is partially due to a lack of standards to inform how microfluidics works in combination with other technologies, like the electronic components of a lab-on-chip diagnostic. Until now, this lack of standards has been a result of commercial microfluidic enterprises failing to adequately demonstrate a need for their technology – but Covid-19 may well have changed that.
For scientists trying to fully understand the virus while developing new vaccines and rapid diagnostic tools, microfluidics has been crucial. Market research company Yole believes the instruments developed for molecular diagnostics, immunoassays, rapid point-of-care tests and high-throughput processes for centralised labs, will continue in use. This is reflected by the prediction in its ‘Status of the Microfluidics Industry 2020’ report that growth of the microfluidics product market will occur at a compound annual growth rate (CAGR) of 14% to reach $24.5bn by 2025. The point-of-care testing (POCT) market alone is expected to reach $24.5m by 2022, expanding at a CAGR of 5.7 %.
Yole analysts predicted in late 2020 that the opening of new opportunities in areas such as travel and workplaces – with rapid passenger or visitor screening – that represent billions of potential tests every year, will be needed to help restart the world’s economy. As countries around the world lifted restrictions put in place to control the spread of SARS-CoV-2, we’ve certainly seen testing for the virus carry on in workplaces, where the risk of transmission is also a financial risk to the business. On top of this, many countries still have testing requirements in place for those wishing to visit, and certain airlines now provide the test as part of their package. Another reason for the increased use of POCT technologies is government support for them, which Yole analysts believe will lead to continued development so that countries are better prepared in case of another future pandemic. With all of this in mind, the diagnostics sector may make the best of this bad situation and turn it into a springboard for growth.
Microfluidics combined with electronics
The advantages of using such tiny fluid volumes are larger than one might imagine. The low sample volume reduces cost and accelerates the time required for analysis. The technology also allows for high controllability, higher resolution and sensitivity, without any requirement for skilled personnel or heavy equipment to operate it, which also brings safety benefits.
So, why might it take a global pandemic to help microfluidics become more than a specialist niche? As Dr Holger Becker, CEO of Microfluidic ChipShop, has described, it is difficult to combine the different modules required to replicate an entire diagnostic workflow in one microfluidic cartridge. In contrast to microelectronics, the modelling of individual elements, such as mixers, capillary stop valves or phenomena-like heat transfer with high precision, find their limits in microfluidic system modelling. The complexity and integration of several components together makes the manufacturing process of such devices intensive and expensive, which is why large-scale production has been so difficult to achieve.
The pandemic gave the world a reason to invest in tackling these issues. Although PCR testing has established itself as the gold standard for the detection of a SARS-CoV-2 infection, it has disadvantages microfluidic technologies have long had the potential to address. As well as being costly and difficult to run, PCR tests take a long time to return results; but by combining electronics with microfluidics, rapid PCR can be performed in transportable microreactors, which is particularly useful for point-of-care (POC) diagnostics. As such, a SARS-CoV-2 infection can be detected significantly more quickly, meaning outbreaks can be controlled more effectively. Some commercial devices for rapid detection of SARS-CoV-2 viruses have been successfully developed based on PCR or isothermal amplification.
American molecular diagnostics company Cepheid has developed a ‘sample-to-answer’ PCR system (Xpress SARS-CoV-2) with an integrated liquid handling cassette, making SARS-CoV-2 detection feasible in 45 minutes (30 minutes for a positive test) when used in tandem with its GeneXpert system. The combination provides results with a sensitivity of 98% and a specificity of 100%. In addition, two portable devices have been developed to enable SARS-CoV-2 testing for home use. One is Lucira’s ‘all-in-one’ LAMP device, Lucira COVID- 19, which can detect SARS-CoV-2 in 30 minutes (11 minutes for a positive test).
The other one is Visby Medical Covid-19 ‘all-in-one’ detection device developed based on continuous flow PCR and capable of SARS-CoV-2 detection in 30 minutes. Another, perhaps even more crucial, application has come into focus in the past year: mRNA vaccines are manufactured with microfluidics. Since mRNA is quickly degraded in the body by serum endonucleases and cannot even pass through the cell membrane due to charge separation, liquid nanoparticles (LNPs) are needed for intracellular transport. Due to their high biocompatibility, potent intracellular transfer, and protection against immune reactions and endonuclease degradation, they are particularly suitable as carriers for mRNA vaccines. Using microfluidic mixing processes, nanoparticles can be produced rapidly (in μs to ms) and with precisely defined properties (for example, size, homogeneity, higher encapsulation efficiencies, and higher reproducibility). Until now, an upscaling of this technique has been a major problem, however, a recent study led by University of Pennsylvania graduate research fellow Sarah J Shepherd introduced a simple, scalable, and parallelised microfluidic device containing an array of 128 parallel channels. With this, a maximum output 100 times greater than that of a single microfluidic channel can be achieved, and the output is directly scalable with the number of channels used.
Great potential
Microfluidic-based electronics have shown great potential in many applications, for example, bio-inspired devices, medical sensing systems, and wearables. During the Covid-19 pandemic, rapid and low-cost microfluidic electronic devices were developed for the detection of SARSCoV- 2 by researchers in the US and Taiwan. In contrast to conventional PCR for virus detection, the presence of the virus can be detected by means of distortions in the electrical signal.
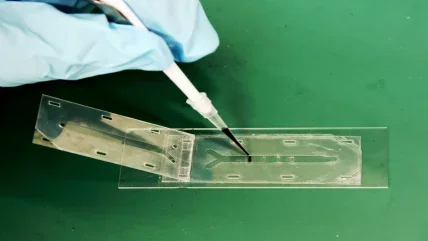
The system developed by the University of Florida and the National Yang Ming Chiao Tung University is based on a metal-oxide-semiconductor field-effect transistor (MOSFET). A disposable test strip is inserted into the MOSFET circuit, which has a microfluidic channel at its tip. This channel consists of clusters of gold-plated electrodes coated with SARS-CoV-2 antibodies, and if a sample positive for the virus is introduced to it, the viral spike proteins bind to the antibodies on the gold electrode. This generates an electrical signal that can be amplified by the MOSFET and sent to the printed circuit board (PCB). Through this method, the system can determine the concentration of the spike proteins and the concentration of the virus particles by the strength of the electrical signal. A wide range of concentrations, from only 100 virus particles per millilitre up to 2,500 virus particles per millilitre in the sample can be detected within one second.
As the PCB is reusable using disposable cartridges, a portable and cost-effective SARS-CoV-2 test system has been developed, which could also be used for the detection of other diseases by coating other antibodies to the gold electrodes. The MOSFET method of these researchers has only been explored in a research setting, and the team behind it are yet to establish sensitivity with an appropriately sized study – but it does give a glimpse of what could be possible by combining electronics and microfluidics in a diagnostic tool. Meanwhile, with the length of time required to obtain a PCR test proving to be a limitation to controlling the pandemic, increasing the availability of testing carried out in portable microreactors could be vital when we’re faced with another virus.
$24.5bn
Expected size of the microfluidics market by 2025, expanding at a CAGR of 14%.
Yole
$24.5m
Expected value of the point-of-care testing (POCT) market by 2022, expanding at a CAGR of 5.7 %.
Yole
Analysing cells using microfluidics
The 13-year-long Human Genome Project (HGP) is heralded as one of the greatest scientific achievements of the past century for mapping the DNA sequence of which every human shares a 99.9% concordance rate. But that remaining 0.1% can account for more than three million differences between one person’s genome and another’s – those differences are called mutations or single nucleotide polymorphisms (SNPs).
Both SNPs and mutations are mistakes made during the replication of DNA – a constantly occurring process – but mutations happen in less than 1% of humans, while SNPs occur in more than 1%. Both, however, can either cause or raise the probability of a person developing a range of diseases, which is why researchers are using microfluidics to isolate specific cells in a process known as total single cell analysis. The hope shared by researchers conducting such experiments is that isolating specific abnormalities in genetic code could shed more light on the ultimate causes of certain diseases, as well as how experimental treatments impact them.
In what could be seen as the next stage of granularity in the understanding of genomics since the HGP reached its conclusion, an international collaborative effort to create a map of the molecular state of cells in healthy human tissues is under way. This, it’s believed, will provide a framework for understanding the differences seen in cells and how they relate to the occurrence and development of human disease. Named the Human Cell Atlas Project, the scientists involved are using microfluidics to process tens and hundreds of thousands of single cells simultaneously to measure their transcriptional profiles at rapidly decreasing costs – bringing the ambitious goal closer to reality every day.






