Metallic surgical implants are a common sight in healthcare, but a scientific paper recently published in the International Journal of Extreme Manufacturing shows that specific metal combinations can significantly reduce post-surgical infections associated with implants. Test results outlined in the paper showed that a novel implant developed by Washington State University researchers killed 87% of bacteria that cause staph infections in laboratory tests.
The objective behind the implant was to find a way to make its surface inherently antibiotic permanent, explains Amit Bandyopadhyay, Boeing distinguished professor at WSU’s School of Mechanical and Materials Engineering and a co-author of the paper. “That meant not adding a dose of medicine to kill the bacteria,” he says. Bandyopadhyay and his fellow co-author, Indranath Mitra, postdoctoral research fellow of physiology and biomedical engineering at the Mayo Clinic, wanted to match or exceed the antibacterial effectiveness of medicine given to a patient after receiving an implant to prevent the formation of biofilm – a layer of bacteria that forms over and encloses medical implants during infection. “Preventing biofilm formation is, at the end of the day, the holy grail everybody’s looking for,” he says.
Major concerns
Bacterial infections related to implants are a major concern for trauma patients in particular, who typically have open, vulnerable wounds related to their injuries. “When there’s an open wound sitting there, it gets infected very fast,” says Bandyopadhyay. Physicians are fully aware that infections can happen during implant surgeries, he adds, “but it’s not that easy to make sure that the site is infection free”.
Bandyopadhyay says up to 30% of fraction management devices become infected after surgery depending on factors, including the type of accident and geographical location where the surgery takes place. “Death due to implant infection is currently at the same level as death due to breast cancer, and is higher than death due to lung cancer,” says Mitra. “It’s predicted by the WHO that by the year 2050 the fatality rate due to implant infection will surpass overall death due to any sort of cancer.”
Currently, the general method for preventing devicerelated infections is by injecting antibacterial medicine or by applying it topically, says Mitra. However, biofilm can still eventually form over the implant even with antibacterial treatments after infection, leaving surgeons no choice other than to remove the implant and then debride the wound area, he says. The process of removing an infected implant can injure healthy muscle and bone, and is especially dangerous for elderly patients.
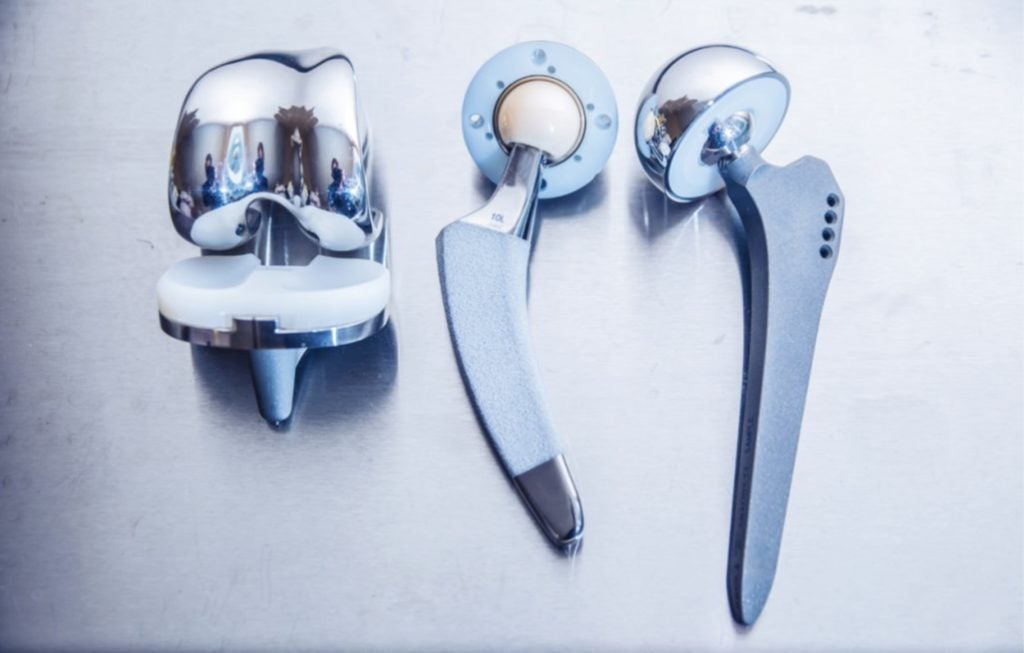
Mitra and Bandyopadhyay’s solution to the problem is an implant constructed with a special blend of copper, which is intrinsically antimicrobial, and tantalum, which supports healthy bone growth and is proven to reduce the loosening of implants. Like conventional implants, the majority of the metal used in the novel implant is titanium, but its use of copper is what gives it its antibacterial properties. “It’s nothing that gets washed away,” Mitra says. “It’s continuously working as long as that implant stays in your body.”
Copper is toxic for bacteria, but also for healthy human cells. But the amount of copper used in the device, which is just 3% of the metal used, is enough to kill bacteria without significantly impacting healthy cells, according to Bandyopadhyay, who says that copper is just half of the solution. “On the second side, we added tantalum, which is the most biocompatible metal. It allows the normal cells to attach better if there is any negative effect from copper towards the normal healthy cells,” he says.
Bandyopadhyay says using a blend of just titanium and copper would kill bacteria and prevent biofilm, but that the implant wouldn’t be able to bond effectively with healthy human tissue. “We want to have good adhesion with the tissue and the implant, but we also want to make sure that if bacteria colonises, it can be resistant.”
Medical implants used in surgeries like knee and hip replacements are kept in place by integrating with bone in a process called “biomaterial mediated healing”, explains Mitra. “When you implant any sort of metals or devices into bone, your aim is that your bone integrates with the material to keep it in place. The first step is for bone cells or tissue to interact with the surface of the material.”
“When you implant any sort of metals or devices into bone, your aim is that your bone integrates with the material to keep it in place.”
Indranath Mitra
Infections disrupt this bonding process by winning what Mitra refers to as a “race to the surface” in which bacteria reach the implant’s surface before healthy cells do. “If the bacteria gets to the surface first, it colonises and covers the surface, and there’s no more space for the bone cells to attach.” The implant’s proprietary blend of copper and tantalum allows healthy cells to win the race to the surface by killing bacteria while simultaneously encouraging bone growth.
Exploring options
Bandyopadhyay and Mitra 3D-printed and tested implants with varying percentages of tantalum and discovered that just 10% delivered the same effectiveness for bone adhesion as devices with 100% coating. The implant’s reduced usage of tantalum, which is significantly heavier than titanium, is particularly useful in load-bearing applications, says Bandyopadhyay.

When implants become infected and need to be removed, physicians typically reflect on how specific procedures within the surgery could have been improved, Mitra says. “But instead of thinking in retrospect while you’re already on the way to the bedside application, take a step back and see if you can do something while the material is still in the bench stage – that’s what we aim to do.”
According to some historians, people used copper to treat wounds as far back as 2,000BC, and scientists have long known about the metal’s antimicrobial properties. This poses the question of why the medical device industry hasn’t explored alternative metal combinations like Bandyopadhyay and Mitra’s. Bandyopadhyay acknowledges the healthcare industry – especially orthopaedic device makers – is slow to adopt new and better technologies, but says that it eventually does.
“In the US alone, we used about 200,000 3D-printed porous metal implants in 2023. We started talking about porous metal implants about 20 years ago, and I still remember my first-generation conversations with various groups and I was discouraged by everyone,” he says, adding that he was told that 3D-printed metallic devices would never be used in the human body. The medical device industry follows news of new technologies very closely, Bandyopadhyay says, but companies typically wait for someone else to take the first step to avoid risk.
Well-funded R&D departments were once a part of most large medical device corporations, notes Bandyopadhyay, but most now employ a different strategy for implementing new technologies. “Their business model is, ‘let’s go ahead and buy the small companies because they have taken the risk, have vetted the ideas, taken a concept to a product line, and now most likely have a device approved’. It’s a lot cheaper for them to buy those small corporations and incorporate their product into their product lines than trying to look at a hundred different ideas and see if one or two of them are making sense or not.”
Bandyopadhyay says he and Mitra are fortunate that their novel implant has proven to be successful and predicts within the next three years we’re likely to see “hundreds” of scientific papers exploring similar concepts. Then, multiple companies in Asia, Europe and the US will explore antimicrobial metals for implants, raise funds and one of them will at least make one product, he predicts. “And once that happens, and once that company is sold for $20, $30, $40 million, you’ll start to see all the large corporations say, ‘okay, fine’.”






