Researchers at the National University of Singapore (NUS) have introduced microneedle technologies designed to improve the healing of diabetic wounds, which often lead to severe complications and amputations.
These persistent wounds impact over 6% of the global population, with Singapore experiencing approximately four lower limb amputations daily due to non-healing diabetic wounds. A study in Singapore found that, in 2017, healthcare costs related to amputations were around S$23,000 ($17,180) per patient.
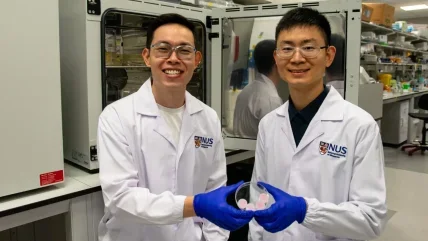
The innovations, developed by assistant professor Andy Tay and his team from NUS’s Department of Biomedical Engineering and the Institute for Health Innovation and Technology, focus on preserving growth factor functions and eliminating harmful inflammatory compounds.
Tay said: “Growth factors are important for wound healing because they regulate key cellular functions. However, in diabetic wounds, these growth factors are rapidly broken down by other enzymes known as proteases.
“This dramatically slows down wound recovery. At the same time, diabetic wounds are characterised by persistently high levels of inflammation.”
The researchers designed microneedles not only for delivery but also for the extraction of compounds to address these issues. The approach is minimally invasive and allows active substances to be directly introduced into wounds.
Tay said: “We wanted to tackle these two issues by using microneedles for both delivery and extraction.”
According to the researchers, traditional growth factor delivery via hydrogel is often ineffective due to rapid degradation in chronic wound environments, necessitating repeated high-dose administration.
The first NUS approach increases growth factor production within the wound. Sucralfate microneedles (SUC-MN) were developed to deliver interleukin-4 (IL-4), stimulating growth factor production in diabetic tissues.
IL-4 aids immune response regulation and tissue regeneration, while sucralfate protects against growth factor degradation. This technique accelerated healing twice as fast compared to conventional treatments.
In a novel exploration, the NUS team utilised microneedles to extract pro-inflammatory proteins and immune cells. To achieve this, they used heparin-coated porous microneedles (HPMN) that act like sponges, absorbing chemokines and monocytes responsible for inflammation.
Their research showed a reduction in tissue inflammation by 50% and wound size by 90% after 14 days.
NUS said that HPMN demonstrates potential as a treatment strategy for inflammatory skin disorders like psoriasis, offering deeper tissue-level intervention compared to existing surface-level treatments. The technology could advance personalised wound care and tailored treatments for various inflammatory conditions.
The researchers team plans further studies to advance these technologies commercially. They aim to refine microneedle pore sizes using advanced techniques such as 3D printing and incorporate antibacterial properties to address infection-associated non-healing wounds. Flexible microneedle patches are also being designed for better adaptability to different tissue shapes.






